Since the outbreak of COVID-19, clinicians have seen a dramatic increase in patients with acute health problems associated with eating disorders.
To tackle the issue, Cornwall Partnership NHS Foundation Trust has partnered with healthcare technology firm Tunstall Healthcare to support young people with eating disorders during the COVID-19 crisis.
The Trust provides both physical and mental health services to children and adults, including young people over the age of 11 with a range of eating disorders, including Anorexia Nervosa, Bulimia Nervosa and Restrictive Eating Disorder.
When the COVID-19 pandemic hit, Tunstall developed a number of schemes to respond to the emergency, offering healthcare providers technology solutions including remote health monitoring, to assist with caring for vulnerable people.
The normal care pathway offered by Cornwall Partnership NHS Foundation Trust includes children living with eating disorders attending a clinic to monitor their vital signs and symptoms. However, due to the restrictions in place during COVID-19 an alternative approach has been developed.
UK managing director of Tunstall Healthcare, Gavin Bashar, says: “We’ve seen many clinics being closed during lockdown with face to face appointments only offered for emergencies due to the risk of cross-infection during COVID-19.
“Although inpatients are continuing where needed, this has been problematic as many wards simply aren’t set up to enable the provision of care while also safely supporting social distancing.”
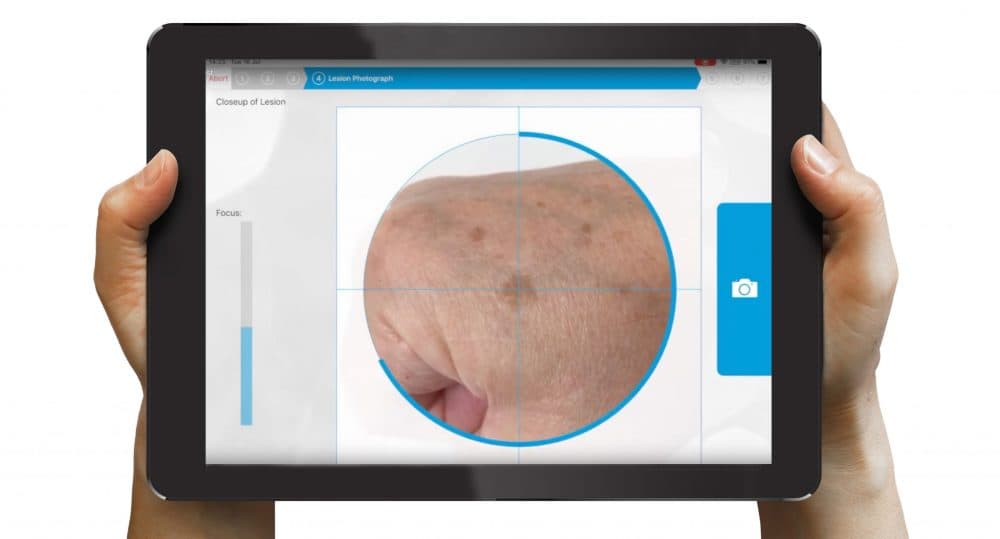
Tunstall Healthcare and the Trust worked together to introduce remote health monitoring for patients, using the myMobile™ app and ICP ‘triagemanager®’ software to enable clinicians to support patients in their own homes and collect patient data.
Patients use devices to take weekly readings of their vital signs including blood pressure, temperature and weight. They are also required to answer a range of symptom-related questions including whether they’ve experienced fainting episodes and if they are able to stand from a squatting position.
Any breaches of parameters set for individual patients raise an alert on the system. Clinicians can then log into a secure portal and ensure patients are prioritised according to the need for intervention. Individual readings can also be viewed over time to monitor progress, with the standard monitoring period expected to be 26 weeks.
Bashar says: “Any delay or interruption to the treatment of adolescents with eating disorders can have serious implications for their recovery, so the rapid deployment of the system has meant that this vulnerable patient cohort has continued to receive support at a time when many are experiencing increased anxiety.”
In other parts of the country, the majority of NHS trusts have turned to video, online or telephone support to cope with the unprecedented circumstances. Bashar says that although these methods have their benefits, they don’t offer the same level of insight as remote health monitoring.
Tunstall is in conversation with other NHS trusts and integrated care systems about deploying similar initiatives to support adolescents with eating disorders during the pandemic.
According to the Oxford NHS Foundation Trust, clinicians have been reporting an increasing number of patients being admitted to hospital with acute cases of malnutrition since the emergence of the pandemic.
The UK’s leading eating disorder support charity, Beat, has reported a 72 percent increase in contact across all its helpline channels in June 2020 compared to February of this year.
Bashar says: “Eating disorders thrive in isolation, and lockdown has had a major impact on the mental health of patients.
“Any changes in day-to-day life and normal routines can be challenging to navigate for adolescents living with eating disorders, and prolonged periods of time spent at home can adversely impact their condition.
“Many people living with eating disorders experience issues around control, and the pandemic has led to feelings of having less control than normal, in turn increasing anxiety and corresponding coping mechanisms.
“We’ve also seen other sources of support such as clinics and counseling not being available in the same way, and more messages in the media about exercising and losing weight which can all negatively impact adolescents living with eating disorders.”
As a result of the initiative, Tunstall Healthcare expects that hospital admissions will be reduced, early intervention will increase, self-management will improve, and patients will benefit from better health and wellbeing.
Vicki Slade, digital health lead at Cornwall Partnership NHS Foundation Trust, added: “The use of Digital Health Technology to support patients is a key part of the novel coronavirus standard operating procedure.
We have been able to use a quality improvement approach so that we can collect and analyse data, to test change. This has allowed us to introduce, develop and refine the service provided to this specific patient group.
Early feedback from clinicians, patients and carers is positive and I hope that we will be able to fully review towards the end of this year this new model of support.”