As the demand for IVF treatment continues to surge, the role of medical technology, or medtech, is proving evermore crucial in the future of fertility…
A little over 40 years ago, when the world’s first IVF baby came into the world, science took a major leap into the future, and couples everywhere were given hope. Science had done it, and it the future of fertility was looking very bright indeed.
Fast forward to 2022, and approximately 1 in 7 couples in the UK have difficulty conceiving. Data shows that nearly 48 million couples experience infertility worldwide. As a result, the demand for IVF treatment continues to surge, with more and more people seeking alternative paths to parenthood.
So how can medical technologies help? What options are available?

Medtech and fertility
Cynthia Hudson, Leading Embryologist and VP of Clinical Strategy at TMRW Life Sciences, spoke to Health Tech World about how medical technologies have a vital role to play in successful fertility.
She said: “Now, an estimated ten million babies are born worldwide using assisted reproductive technologies, with IVF one of the most popular forms of modern breakthroughs.
“In fact, IVF birth rates in 2019 were three times higher than they were in 1991, due to rising rates of infertility, trends towards delayed family planning and its increasing popularity as a result of the high success rates.
“This is great news for the increasing numbers of patients seeking treatment. Years of research and development have resulted in better lab equipment, stimulation medications, as well as improved techniques and tools used by clinicians, all with the aim of making sure patients can go through as few treatments – which can be very emotionally and physically challenging – as possible to achieve parenthood.
“In fact, looking ahead, it is likely that in the near future, as many as 10% of all children will be conceived through IVF in many parts of the world.”

Assisted Reproductive Technology (ART)
Some couples will get pregnant quickly with no struggle, for others, it can take much longer.
Couples are advised to see a doctor if they have not conceived after around a year of trying (or six months of trying for women over 35 years of age*).
A couple might struggle with infertility for a variety of reasons – this could include medical conditions such as endometriosis, problems with sperm production or genetic disorders, but also lifestyle factors e.g. age, weight, smoking, alcohol intake, and stress.
And while in some cases infertility is not always treatable, there are still options available due to the capabilities of modern medicine and technology.
For anyone struggling to conceive with their partner, tackling fertility issues usually starts by seeing a doctor who can run tests and try to determine a cause – although, this sometimes remains inconclusive. Whether or not a specific diagnosis is identified, the treatment and path to parenthood often involves some form of Assisted Reproductive Technologies (ART).
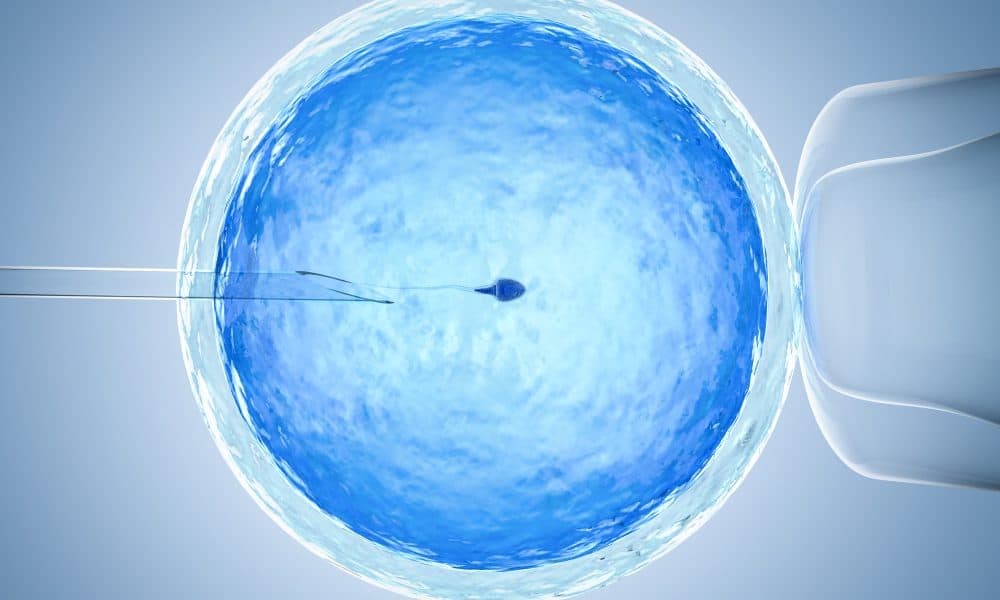
Assisted Reproductive Technology treatments are an option available to those needing support conceiving. In short, ART refers to high-tech treatments that facilitate the meeting of eggs and sperm, either in vitro or in vivo, to increase the chances of achieving a pregnancy.
There are several types of ART available and choosing the right option will depend on the reasons why an individual or couple is struggling to get pregnant in the first place.
This includes ICSI (intracytoplasmic sperm injection), IVF, and IUI (intrauterine insemination).
ART treatments begin by processing sperm produced either by ejaculated semen or by a needle from the testicle. This can be from the person seeking parenthood, or from a donor, depending on the circumstances.
Next, the samples are processed and introduced to the eggs. Here are some of the ways this can take place:
Intrauterine insemination (IUI)
Placing sperm into a woman’s womb around the time of ovulation. Medicines are usually given to the woman first to increase the number of eggs released, thereby increasing the chances of conception. This method can benefit those in same-sex relationships, have irregular periods, or patients struggling to have sex or maintain an erection.
In-Vitro Fertilisation (IVF)
Mixing sperm with multiple eggs in the laboratory. The resulting embryo can then be placed into the uterus. This method is more invasive than IUI since the eggs need to be collected and processed, but it is also highly effective and can be used in almost any circumstance to attempt pregnancy.
It is particularly useful for those using a third or fourth party to help them conceive, women with blocked fallopian tubes, those using a gestational carrier, or those using donor eggs.
IVF also allows for the testing of embryos for genetic diseases or other chromosomal abnormalities. Not all embryos that are transferred to the uterus will result in a live birth, but there are techniques that embryologists can use in the lab to try to pick the best ones to put back.

Intracytoplasmic Sperm Injection (ICSI)
With ICSI, a single sperm is injected through a tiny needle into an egg to attempt to fertilise it in the laboratory, which is then transferred into the uterus.
Your doctor may recommend using ICSI in an IVF cycle if there is a low sperm count, frozen eggs are being used, or if regular IVF was unsuccessful. ICSI is also sometimes used in cases where genetic testing of the embryos is required.
Medtech & the future of fertility
Cynthia continued:
While IVF has totally redefined the ability of the human species to procreate, fertility clinics are facing real challenges keeping up with the huge demand, and the labour intensive manual systems that haven’t been updated in decades simply cannot cope.
This is where innovation is urgently needed.
The problem is, despite the rapid growth and demand for IVF, the tools fertility clinics use to manage and track these frozen eggs and embryos have remained largely unchanged since IVF was first adapted from livestock breeding more than 40 years ago.
Patients are now freezing their eggs and embryos at higher rates than ever before, which clinics have struggled to keep up with, given that they were never designed to be long-term cryo (storage) banks.
And this brings huge risks and inefficiencies that are holding many clinics back, preventing them from helping all of the increasing numbers of couples looking for support.
Currently, the process embryologists use to keep track of and manage the frozen eggs in the dewars over time involves a reliance on manual and analogue identification, tracking, and written record keeping.
While this method was manageable with a few hundred patients, the process has become enormously time consuming and riddled with risk as the numbers have risen into the thousands.
Keeping track of everything by hand is not scalable or sustainable. There are common instances of specimens being labelled by hand and client data being held in insufficiently secure systems.
As a result, these error-prone processes have led to some unfortunate incidents where precious eggs have been lost, or the wrong embryos have been transferred into patients. In fact a recent survey found 27.8% of embryologists reported being unable to locate, identify, or were unsure of specimens in their storage facility (Source: TMRW survey of ~300 embryologists conducted in March 2020.)
Simply put, the backend infrastructure isn’t keeping pace with the demand, leaving room for error and taking embryologists away from what they do best – supporting patients through one of the toughest times in their lives and focusing on the science rather than record keeping and admin.
Tech if changing IVF
TMRW Life Sciences is changing these processes through advanced technology, and has created a platform that automates the unique identification, tracking and tracing of frozen eggs and embryos in order to reduce errors and increase efficiency. They are replacing traditional dewars with a robot, and can now, using software, digitally track and remotely monitor tens of thousands of patient specimens 24/7 to avoid losing, misidentifying, or damaging the cells.
With the projected number of IVF births rising, clinics need to embrace modernisation with scalable solutions that can improve efficiency, meet demands, and future-proof the IVF process.
Clinics must invest in innovations, like the specimen-management platform created by TMRW, to offer their doctors, embryologists and patients greater reassurance and peace of mind through automated, safer and more sophisticated IVF care.
This is the next frontier for fertility.
Don’t miss…






