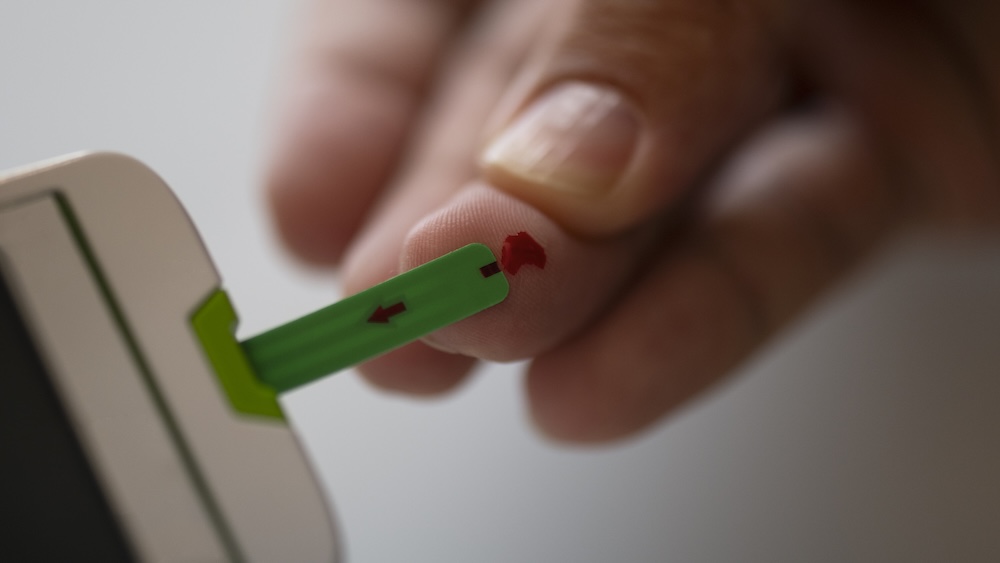
A finger-prick test is being trialled in the UK, US and Canada to see if it can help diagnose Alzheimer’s disease in people aged over 60.
The study involves 1,000 volunteers and will look for biomarkers linked to Alzheimer’s by analysing blood from a simple finger-prick.
Biomarkers are measurable signs in the body, and researchers will measure proteins linked to the disease.
The Bio-Hermes-002 study is led by medical research charity LifeArc and the Global Alzheimer’s Platform Foundation, with support from the UK Dementia Research Institute.
Dr Giovanna Lalli, director of strategy and operations at LifeArc, said: “We are looking at the presence of three proteins that have been linked to Alzheimer’s disease, so-called blood-based biomarkers.
“By analysing the concentration and the levels of these proteins it may tell us whether a person is at risk of developing Alzheimer’s disease.”
Studies have shown proteins called amyloid and tau can build up in the brain more than 15 years before symptoms appear. Alzheimer’s is the most common form of dementia.
All volunteers will also have current standard tests, either a specialised brain PET scan, which uses a radioactive tracer, or a lumbar puncture to take a sample of cerebrospinal fluid from the spine.
These tests can be expensive, time-consuming and invasive, with only two in 100 Alzheimer’s patients offered them, so the finger-prick test could change how the condition is identified.
With tests not currently widely available across the UK, Professor Fiona Carragher, chief policy and research officer at the Alzheimer’s Society, said: “getting an accurate diagnosis takes far too long”.
She added: “With new treatments on the horizon, early and accurate diagnosis must be a priority for the NHS.
“That’s why we’re funding work to bring blood tests for dementia to the NHS, so everyone who would benefit from a diagnosis can get one quickly and accurately.”
Dr Michael Sandberg, a London GP, took part after seeing his mother’s decline from Alzheimer’s.
He told the BBC: “My mother did very well on a trial and that encouraged me to take part.
“I believe knowledge is power and am really excited that you may be able to screen people at risk of dementia without expensive scans or needles.”
When Sandberg received his results, both the brain scan and the finger-prick test were negative.
He said: “It’s a huge relief, knowing what my mother went through”.
Scientists will need to analyse findings from all 1,000 volunteers before they know how useful the finger-prick test is at spotting Alzheimer’s risk.
Dr Emer MacSweeney, a neuro-radiologist at ReCognition Health who is recruiting some of the UK volunteers, said: “If this is successful, it provides a ubiquitous, accurate test which can detect the presence of abnormal amyloid protein in the brain without complicated, expensive investigations.”
Using biomarkers in the blood to identify Alzheimer’s risk is a fast-moving area of research.
Last year US regulators approved a blood test for diagnosing Alzheimer’s, though it uses a traditional blood draw with a needle and syringe.
Another UK study is under way looking at whether blood tests improve diagnosis and treatment in real-world settings.
One advantage of the finger-prick approach is that people could do it at home and post the sample to a lab for analysis, as it does not need refrigeration.
There are hopes blood tests could eventually be used to screen older adults for dementia.
So far, 883 of the 1,000 participants have enrolled, with more than 360 completing all tests.
The group includes cognitively normal people, those with mild impairment and some with early-stage Alzheimer’s.
At least 25 per cent of volunteers will be from under-represented groups.
The trial is expected to complete in 2028.