A bionic pancreas is more effective at managing type 1 diabetes than standard insulin delivery methods, a new study has found.
The device uses next-generation technology to automatically deliver insulin to patients with the condition.
Automatic insulin delivery systems, also known as artificial pancreas and closed-loop control systems, track blood glucose levels to automatically deliver insulin when required.
These systems replace reliance on testing glucose levels by fingerstick, continuous glucose monitoring or pump without automation.
The bionic pancreas requires less user input that other artificial pancreas technologies and also delivers more automation, with the device’s algorithms continually adjusting insulin doses automatically based on users’ needs.
Users initialise the system by entering their body weight into the device’s dosing software at the time of first use.
Users of the bionic pancreas also do not have to count carbohydrates, nor initiate doses of insulin to correct for high blood glucose levels.
Meanwhile, health care providers do not need to make periodic adjustments to the settings of the device.
Dr. Guillermo Arreaza-Rubín, director of the National Institute of Diabetes and Digestive and Kidney Diseases diabetes technology program, said:
“Keeping tight control over blood glucose is important in managing diabetes and is the best way to prevent complications like eye, nerve, kidney, and cardiovascular disease down the road.
“The bionic pancreas technology introduces a new level of ease to the day-to-day management of type 1 diabetes, which may contribute to improved quality of life.”
The 13-week trial enrolled 326 participants ages 6 to 79 years who had type 1 diabetes and had been using insulin for at least one year.
Participants were randomly assigned to either a treatment group using the bionic pancreas or a standard-of-care control group using their usual insulin delivery method.
All control group participants were provided with a continuous glucose monitor, and nearly one-third of the control group were using commercially available artificial pancreas technology during the study.
In the bionic pancreas group, glycated hemoglobin, a measure of a person’s long-term blood glucose control, improved from 7.9 per cent to 7.3 per cent, yet remained unchanged among the standard-of-care control group.
The bionic pancreas group participants spent 11 per cent more time, approximately 2.5 hours per day, within the targeted blood glucose range compared to the control group.
The results were similar among youth and adult participants, and improvements in blood glucose control were greatest among participants who had higher blood glucose levels at the beginning of the study.
Dr. Steven Russell, study chair, associate professor of medicine at Harvard Medical School, and staff physician at the Massachusetts General Hospital in Boston, said:
“Our observation that this system can safely improve glucose control to the degree we found, and do so despite requiring much less input from users and their health care providers, has important implications for children and adults living with diabetes.”
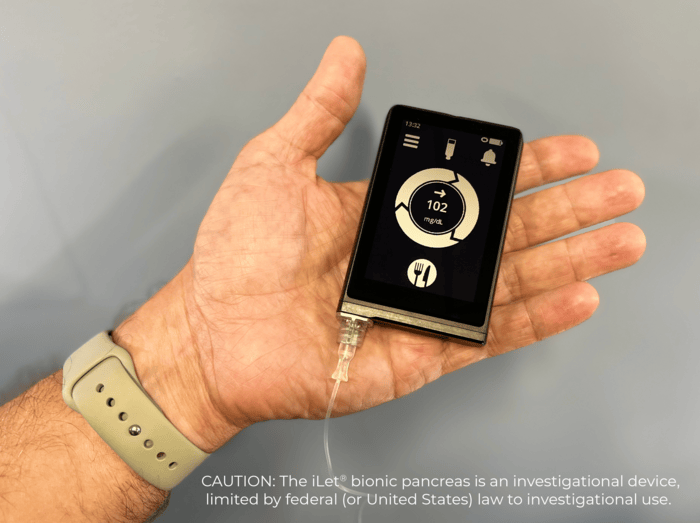
Image: Beta Bionics








