AI can identify which patients need treatment to prevent vision loss, study finds
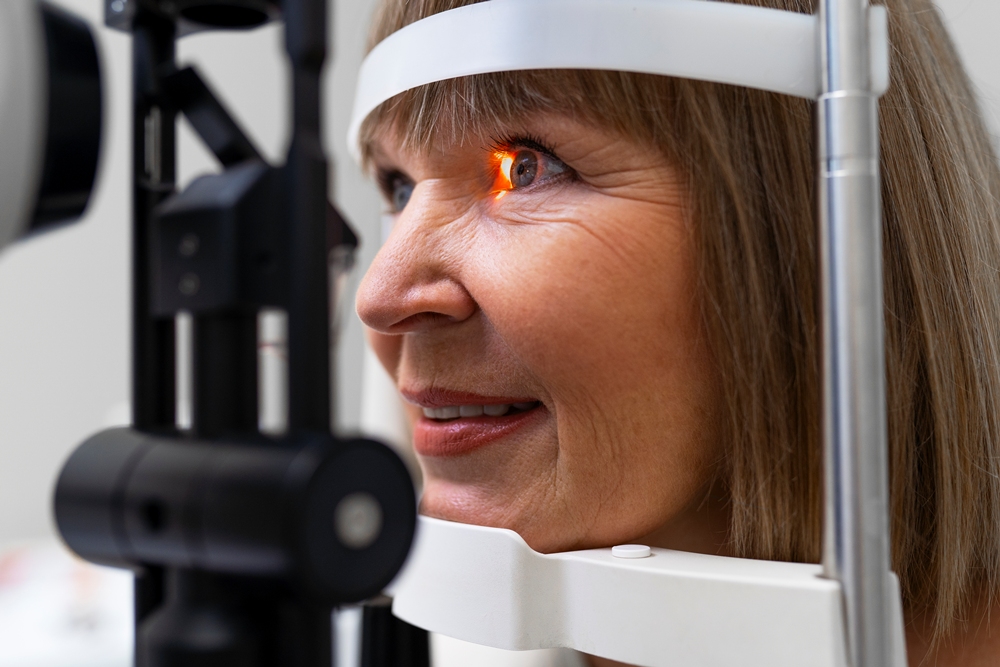
Artificial intelligence can help spot which patients with keratoconus need early treatment, avoiding years of routine monitoring, new research has found.
An AI algorithm analysed 36,673 eye scans from 6,684 patients to determine who needed urgent cross-linking treatment and who could be safely monitored.
The system placed around two-thirds of patients into a low-risk group needing only monitoring, while one-third were flagged as high-risk and requiring prompt cross-linking.
When data from a second hospital visit was added, the algorithm successfully sorted up to 90 per cent of patients.
Dr Shafi Balal of Moorfields Eye Hospital NHS Foundation Trust and University College London (UCL) said: “In people with keratoconus, the cornea – the eye’s front window – bulges outwards.
“Keratoconus causes visual impairment in young, working-age patients and it is the most common reason for corneal transplantation in the Western world.
“A single treatment called ‘cross-linking’ can halt disease progression.
“When performed before permanent scarring develops, cross-linking often prevents the need for corneal transplantation.
“However, doctors cannot currently predict which patients will progress and require treatment, and which will remain stable with monitoring alone.
“This means patients need frequent monitoring over many years, with cross-linking typically performed after progression has already occurred.”
Keratoconus affects up to 1 in 350 people, usually starting in teenage years or early adulthood.
In mild cases it can be managed with contact lenses, but in severe cases it may progress rapidly, sometimes leading to corneal transplant if untreated.
At present, doctors cannot reliably predict who will deteriorate. This means patients often need long-term monitoring.
Cross-linking, a one-off procedure using ultraviolet light and vitamin B2 drops to stiffen the cornea, can stop disease progression and is effective in more than 95 per cent of cases.
The researchers used AI to study optical coherence tomography (OCT) scans – detailed images of the cornea – alongside patient data.
The algorithm predicted from the first visit whether a patient’s keratoconus would worsen or remain stable.
Dr Balal said: “This is the first study of its kind to obtain this level of accuracy in predicting the risk of keratoconus progression from a combination of scans and patient data, and it uses a large cohort of patients monitored over two years or more.
“Although this study is limited to using one specific OCT device, the research methods and AI algorithm used can be applied to other devices. The algorithm will now undergo further safety testing before it is deployed in the clinical setting.
Our results could mean that patients with high-risk keratoconus will be able to receive preventative treatment before their condition progresses.
“This will prevent vision loss and avoid the need for corneal transplant surgery with its associated complications and recovery burden.
“Low-risk patients will avoid unnecessary frequent monitoring, freeing up healthcare resources. The effective sorting of patients by the algorithm will allow specialists to be redirected to areas with the greatest need.”
The team is now developing a more advanced AI model trained on millions of scans, which could also be used to predict keratoconus progression, detect eye infections and identify inherited eye diseases.